Introduction
General practice in England is facing an unprecedented level of pressure. With an increasing patient load, staff shortages, and mounting administrative demands, healthcare professionals in GP surgeries are also dealing with another critical issue: a rise in challenging and aggressive behaviour from patients and the public.
While physical violence is a significant concern, verbal abuse, threats, and intimidation are also creating a stressful and often unsafe working environment. This article explores the types of challenging behaviours that general practice staff encounter, the impact on healthcare professionals, and practical de-escalation strategies, including the Kaplan & Wheeler Model, to support those on the frontline.
The Growing Challenge: Abuse in General Practice
Recent reports highlight a disturbing trend: increasing aggression and abuse towards general practice staff. A British Medical Association (BMA) survey found that nearly 75% of GPs and their teams have faced verbal abuse, while 15% reported incidents of physical violence. This rising hostility is not limited to face-to-face interactions; many staff members also experience online abuse, particularly through social media and patient feedback portals.
Some common types of challenging behaviour seen in general practice include:
- Verbal Abuse: Swearing, shouting, or making derogatory remarks towards receptionists, nurses, or GPs.
- Threatening Behaviour: Patients making intimidating comments, gesturing aggressively, or directly threatening staff.
- Physical Violence: Incidents of pushing, hitting, spitting, or throwing objects at staff.
- Passive-Aggressive Behaviour: Patients repeatedly making sarcastic or undermining comments, deliberately causing disruptions.
- Emotional Outbursts: Individuals in distress or frustration raising their voices or refusing to engage in conversation constructively.
- Demanding and Unreasonable Behaviour: Patients expecting immediate attention, ignoring appointment protocols, or refusing to accept waiting times.
- Online Harassment: Negative and sometimes threatening comments on social media, emails, or online review platforms.
These behaviours not only create a challenging work environment but can also lead to increased stress, burnout, and a decline in staff retention rates within the NHS.
The Kaplan & Wheeler Model: Understanding the Stages of Aggression
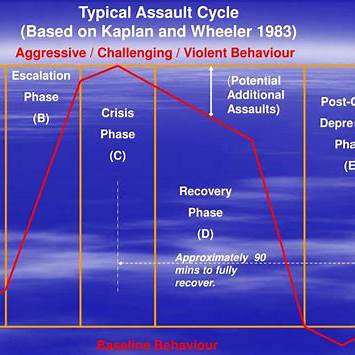
One effective way to manage challenging behaviour in a healthcare setting is by understanding the cycle of aggression. The Kaplan & Wheeler Model identifies five key stages in the assault cycle, providing a framework for recognising early warning signs and intervening before situations escalate.
- Trigger Phase – This is the initial stage where a person experiences frustration, distress, or anxiety due to an external factor (e.g., long waiting times, perceived unfair treatment, or a personal crisis). Early intervention at this stage can prevent escalation.
- Escalation Phase – At this point, signs of aggression begin to emerge. Patients may raise their voice, become increasingly argumentative, or display hostile body language.
- Crisis Phase – This is the peak of aggression, where physical violence or serious verbal threats may occur. Staff safety becomes a priority, and crisis management techniques should be applied.
- Recovery Phase – After the crisis, emotions begin to settle. The person may feel guilt, remorse, or exhaustion.
- Post-Crisis Depression Phase – The individual might experience shame or regret, making this a key moment for debriefing and discussion.
By recognising these stages, general practice staff can implement timely interventions to de-escalate situations before they reach a crisis point.
Top Tips for De-Escalation in General Practice
When confronted with challenging behaviour, staff should be equipped with effective de-escalation strategies to manage situations safely and professionally. Here are some top tips for diffusing aggression in a GP surgery:
- Stay Calm and Professional – Keep your tone steady, avoid responding emotionally, and maintain a composed body posture. A calm approach can help prevent further escalation.
- Use Active Listening – Show empathy by listening carefully, nodding, and repeating back key concerns to demonstrate understanding. Often, patients just want to be heard.
- Acknowledge Their Feelings – Saying phrases like, “I understand that this situation is frustrating for you” can validate their emotions and help de-escalate tension.
- Set Clear Boundaries – Politely but firmly set expectations: “I want to help you, but I need you to lower your voice so we can discuss this properly.”
- Offer Solutions Where Possible – If appropriate, suggest alternatives or compromises to address their concerns.
- Use Non-Threatening Body Language – Avoid crossing arms, standing too close, or making sudden movements that could be perceived as hostile.
- Know When to Seek Help – If a situation is escalating beyond control, call for support from a manager or security personnel to ensure staff safety.
- Follow Up When Necessary – If a patient has calmed down after an outburst, checking in later can help rebuild rapport and prevent future incidents.
- Implement Staff Training on Conflict Resolution – Regular training in de-escalation techniques, including role-playing scenarios, can empower teams to handle difficult situations more effectively.
- Encourage Incident Reporting – Ensure that all instances of abuse or aggression are logged to identify patterns and improve workplace safety measures.
Conclusion
The pressures facing general practice in England extend far beyond clinical care. Dealing with challenging behaviour is now an everyday reality for NHS staff, making conflict resolution skills more vital than ever.
By understanding aggression through models like Kaplan & Wheeler and implementing effective de-escalation techniques, healthcare professionals can create a safer, more supportive environment for both staff and patients. Ongoing training, clear policies, and a zero-tolerance approach to abuse will be key in protecting those who dedicate their careers to caring for others.
If you’re interested in conflict resolution training tailored for general practice, Good Sense has been working with the NHS since 1996, equipping frontline healthcare teams with the skills they need to manage challenging interactions effectively. Get in touch to learn how we can support your practice.

Recent Comments